Blog Posts
Words Matter: The Importance of Positive Environment and Affirmations in Labor
Last week I saw a quote attributed to neuroanatomist Dr. Jill Bolte Taylor that said, “Please take responsibility for the energy you bring into this space.” While I was thinking to myself “Yes! We all need to do that”, my partner was looking over my shoulder saying aloud “That’s snarky.” It was a curious moment in which our perception and response to these words was completely different. I was thinking about labor and how easy it is to affect a labor simply by changing the energy in the room and the words we use. He was thinking...something different.
Research shows that it takes between 5-10 positive comments to neutralize a negative one. This is in part due to the fact that our brains process negative experiences and comments more thoroughly, and in a different part of our brain, than positive experiences and comments. This results in us being able to remember the negative events more clearly and in more detail, to respond more strongly or viscerally, and to resist reclassification of the experience as a positive. For example, all of us know how difficult it is to reverse a bad first impression. Negatives have a greater potential to sink in and stick, even in people who are otherwise positive thinkers. This is why keeping a positive environment and using positive affirmations is critical in the birthing room.
Well meaning supporters, whether family, friends, or care provider staff, often express empathy in ways that undermine a person’s will in labor. Statements like “you don’t have to be a superhero”, “there’s no prize for doing this without pain medication”, “you don’t have to work so hard” seem innocent enough. They all however, almost always, forget a critical ending to the sentence: “if you don’t want to”. “You don’t have to work so hard if you don’t want to.” It’s important to know IF a person wants to. If they want to work hard, be a superhero, get the prize of self-satisfaction, etc. their supporters should cheer them on and support their determination. It's just as easy to say “you’re a superhero", “go for your goal and get that prize”, and “it’s hard and you can do this”. So, say that instead.
Worse than the words that undermine will are the ones that undermine ability and plant seeds of doubt. By its natural design, labor elicits its own hormonal rushes which can stimulate a fight or flight response, that is, times in which one has to decide if they can do it or if labor needs to stop to get to a safer place. At those times, especially during what I sometimes call “transition talk”, it’s common to hear “I can’t do this.” The right response to this statement should lift a person up and give them strength and belief in their abilities. It is “yes, you can,” not “I don’t think you can either.” That should be obvious, right? But sometimes the response isn’t as blunt as that, and yet it still implies the same thing.
Many doulas have found themselves having to diffuse doubt bombs left by strangers, friends, family, and care providers early in labor or perhaps long before labor even began. I don’t think I’ve ever had a client planning a non-medicated labor who didn’t have at least one person express uncertainty about it (which is often followed by their own negatively charged and sometimes scary story). Hopefully, not everyone has to deal with more serious doubt bombs, but many do. These are comments such as remarking that a baby is possibility being too big or a pelvis is possibility too small. While these again are usually well meaning comments, meant to prepare someone for what another might think is the likely or inevitable conclusion, nothing is ever inevitable until the conclusion itself has played out.
 If you’re a care provider and you’ve ever once thought it was helpful to tell someone working hard in early labor that “baby might not want to come out that way,” please reconsider and instead encourage her to walk or lunge, or just offer a positive affirmation or a cool cloth. If you’re a care provider and you’ve ever thought saying “this room is cursed, everyone ends up with cesareans in here” is useful knowledge to a person in labor, please rethink your encouragement strategies. When people infuse negativity and doubt into a birthing environment, it changes the entire dynamic of a labor. Words, even looks or posture, have the tremendous power to get someone to stop thinking “I can do this” and starting thinking “maybe I can’t do this.” No one should have to labor like that. No one should have to prove they can to anyone but themselves. Use your words wisely. Take responsibility for the energy you bring into this space.
If you’re a care provider and you’ve ever once thought it was helpful to tell someone working hard in early labor that “baby might not want to come out that way,” please reconsider and instead encourage her to walk or lunge, or just offer a positive affirmation or a cool cloth. If you’re a care provider and you’ve ever thought saying “this room is cursed, everyone ends up with cesareans in here” is useful knowledge to a person in labor, please rethink your encouragement strategies. When people infuse negativity and doubt into a birthing environment, it changes the entire dynamic of a labor. Words, even looks or posture, have the tremendous power to get someone to stop thinking “I can do this” and starting thinking “maybe I can’t do this.” No one should have to labor like that. No one should have to prove they can to anyone but themselves. Use your words wisely. Take responsibility for the energy you bring into this space.
Use words that encourage:
- You’re making progress
- You’re doing great
- You’ve got a right to be proud of yourself
- You’re a wonderful mother/parent/person
- I’m here for you
- I love you
- I’m proud of you
- You’re beautiful
- You’re amazing
- You’re strong
- You’re powerful
- I know you can do this
- You know you can do this
- You can do this
17 Tips for Reducing Your Chance of a Cesarean
Here are some tips that we have noticed help improve a low risk birthing person's chances at having a vaginal delivery.
- Visualize the birth you want.
- It's difficult to know or achieve the kind of birth you want if you don't spend some time thinking about your preferences.
- Statistically, women who are unable to visualize a vaginal birth have a higher incidence of cesarean.
- Listen to a guided visualization of a vaginal birth if you have trouble imagining it.
- Choose the kind of birth location that matches the kind of birth you want.
- Does your birth location specialize in the kind of birth you want?
- If you want an unmedicated or low intervention birth, for example, inquire as to how often birthing persons have unmedicated or low-intervention births at that facility during your walk-through. If that number is low, your care facility does not specialize in your preferred type of birth. Be aware that you may be choosing an scenario with which your facility might not have extensive experience and that this may understandibly push them outside their comfort zone. You may have to advocate strongly for your preferences in such an environment.
- Check the cesarean rates of your care facility. Studies show that the chance of having a cesarean depends more heavily on where you deliver than on the provider and you. In California, you can look here.
- Choose a care provider who specializes in the kind of birth you want.
- Midwives are natural birth specialists, trained in physiologic, vaginal birth who will screen patients and pass high risk patients onto surgical specialists.
- OBs are surgical specialists, some of whom are very open in saying they prefer cesarean to vaginal delivery and encourage everyone to have surgery. It's ok to ask what their favorite kind of delivery is. If 30-50% of your OB's patients have a surgical delivery, and only 5% of their patients have non-induced, non-augmented, non-medicated vaginal deliveries, then they don't see natural birth often and may not be very experienced or comfortable with physiological birth. This dynamic of decreasing experience significantly contributed to the loss of breech vaginal delivery options and the rising cesarean rate nationwide.
- It's ok to ask a lot of questions about your care provider's practice, so there are not unexpected surprises when you are in labor. If you are trying for a vaginal birth after a cesarean, for example, you can ask about their success rate with VBACs or even vaginal births in general. Ask how often they induce non-VBACs and if they induce VBACs at all.
- If your care provider says they only do cesareans when necessary, ask them how often they typically see a cesarean as necessary. Do they primarily do them when there may be a potential (but not presently) urgent need in 12-24-48 hours, when the need is currently urgent, or when the need is emergent? Do they do often do cesareans without a trial of labor, and if so, for what reasons? Does their comfort level with the risks match yours?
- Do not put yourself in the position of having to fight for the birth experience you want in a care facility or with a care provider you do not trust. For oxytocin to flow, for the uterus to contract well, and for the cervix to open easily, you need to feel safe and supported.
- If you feel that your care provider is not supportive of your birth preferences (even if they seem very nice, very capable, were your best friend's provider, have been your care provider forever, or were your care provider for a previous delivery), it is 100% ok to find another care provider who is on board and excited about the kind of labor and delivery you're hoping for.
- Most people do not have the energy to ask for pros and cons of recommendations or the ability to thoroughly choose among them in the thick of labor. You need to trust that your care provider is making decisions based on you and your baby, not their own schedule. Conflict with your care provider(s) increases adrenaline, which can then force the lower band of uterine muscle to constrict and keep the cervix closed.
- Travel if you have to.
- Be aware that the most common time for cesareans to be performed is right before a shift change.
- Failure to progress is the #1 reason that labors end in cesarean. In recogizing that care providers may be recommendating cesarean for a "Failure to Progress" prematurely, in 2014 the definition of active labor was changed from 4cm to 6cm. This may help prevent what some have snidely termed "failure to have patience".
- Make a plan for an unmedicated birth. An unmedicated labor helps with dilation, effacement, descent. An upright labor statistically will progress more quickly.
- You need concrete skills to achieve the goal of unmedicated birth. Most people who say they will go with the flow and try to "go natural" without having a skill set to do so, will get an epidural.
- Why should you try to avoid an epidural? First an epidural is a package deal. Required in the package:
- IV fluids
- Continuous fetal monitoring
- Blood pressure cuff
- Bladder catheter
- Restricted positions in bed
- No food or drinks,ice chips only
- Decreased gravity pull on baby
- Possible effects of the epidural package:
- Pitocin for slowed labor
- Less engagement and assistance from baby
- Compressed pelvic outlet making less room for baby to travel through the boney structure
- Cesarean for failure to progress
- Vacuum assistance because fetal ejection reflex is inhibited
- Delivering on hands and knees or upright position helps make more space in the pelvis for baby to come through.
- Take a natural birth childbirth preparation course.
- Note that many hospital classes are often patient preparedness classes and are not primarily focused on helping you develop strategies for an unmedicated birth. Some hospital class instructors aren't allowed to mention risks associated with interventions.
- Statistically, taking a stand-alone class can increase rates of unmedicated birth substantially (example from Birth Boot Camp: 70% have unmedicated births, 30% have medicated births). Many of our local hospitals have a 90-95% epidural rate.
- Hire a doula.
- ACOG noted in 2014 that the single most important thing you can do to lower your risk of cesarean is to hire a doula. Studies show a 50% decrease in cesarean, as well as decreases in need for medications, assisted deliveries, and increases in maternal satisfaction with birth experience, maternal/baby bonding, and breastfeeding rates.
- Say no to non-medically necessary inductions and let the baby choose their birthday. Inducing increases the risk of a primary cesarean. It can also lead to low heart rate, infection, umbilical cord problems, uterine rupture, and hemorrhage postpartum.
- If your care provider is encouraging induction, know your Bishop Score. Scores under 5 are not favorable for induction without cervical ripening and very frequently lead to cesarean. Scores over 10 are considered more favorable for induction.
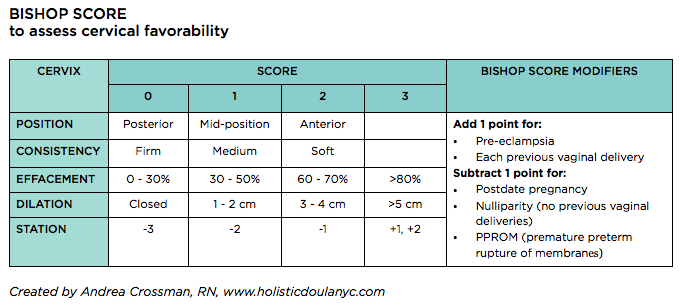
- If your care provider is encouraging induction, know your Bishop Score. Scores under 5 are not favorable for induction without cervical ripening and very frequently lead to cesarean. Scores over 10 are considered more favorable for induction.
- Be active before labor.
- People who are sedentary in pregnancy are 4 times more likely to have a cesarean.
- If you are low risk, many care providers recommend that you stay home until you are in active labor if you're close to the hospital and are expected to have a typical length labor, if that helps you feel more relaxed.
- Taking a class that focuses on the holistic view of what active labor looks like will help you better identify when you're in active labor without checking your cervix.
- Shut down negativity.
- Keep yourself inside a bubble of peace. Your friends, family, and/or complete strangers may view your pregnant belly as an opportunity to process their own birth experience. You are under no obligation to listen. Simply say, "no thank you."
- Get involved in your local ICAN chapter, read Ina May Gaskin, and find positive stories of people who have had beautiful birth experiences.
- If you're having trouble finding ways to think positive, seek support from a therapist, other care provider, or other healer who specializes in birth trauma. There is help out there. We are happy to offer some recommendations.
- Focus on nutrition.
- A well-nourished and hydrated body works through labor more easily. The uterine muscle can contract more effectively. Perineal tissues tear less easily.
- Get your partner on board with your plan, so they aren't coming at this from a place of fear. If they aren't comfortable, you'll be worried about them, not you.
- Be active in active labor. Use movement. Your body communicates with you throughout labor, sometimes using pain to tell you when baby isn't lined up right. Move your body to move the baby.
- Know your options for movement in labor at your chosen care facility. For example, if you have to have continual fetal monitoring, ask for a wireless telemetry unit so you can move away from the bedside.
- Keep things out of your vagina to decrease infection risks. Medical intervention and augmentation have their place, but in the absence of medical need, discuss with your care provider to possibility of:
- Avoid routine cervical checks
- Avoid routine sweeping membranes or stretching the cervix unless actively trying to start or augment labor
- Avoid artificially rupture of membranes
- If baby is breech, check your options for breech vaginal delivery (locally, breech delivery is possible at UCSF and UC Davis) – mybreechbaby.org.
- Be active about getting baby to turn beforehand using the techniques at spinningbabies.com, acupuncture and moxibustion, Webster technique chiropractic care, etc.
- Lastly, remember that no one is promised an uncomplicated birth. Prepare for any outcome.
- Know that it's ok to mourn the birth you didn't get.
- Reach out for support from friends, family, care providers, or organizations like ICAN or Postpartum Support International. We host support meetings for both at our office in Mtn. House. See our calendar for upcoming dates.

Getting Ready for Parenthood: Beyond the birth
If you're like many of our clients, you've invested a lot of time into preparing for having a baby. Friends and family may have done their share to welcome baby by presenting gifts of clothes, toys, and necessities. You've gone about nesting and finding just the right place for everything. All the diapers are neatly stacked and waiting by the changing table. All the clothes are washed, folded, and put away (unless you listened to your doula who said to wash only what you need for the first two weeks and keep the tags on the rest, in case baby grows out of that size before he or she has had a chance to wear every outfit). But what about you? Have you gotten your home ready for the postpartum you? If not, we have a few tips for preparing your spaces.
The Nursing Nook
If you've purchased a rocking chair where you plan to nurse, don't be too disappointed if its most common use is as a gathering spot for dirty clothes or clothes that need to be folded or put away. Many moms don't want to be isolated from the family, hidden in the baby's room every two hours to nurse. Prepare yourself instead to have a mobile nursing kit to bring to whatever spot in which you may find yourself nursing -- the sofa, the living room floor, the kitchen table, your bed, the bathroom (yes, most moms will eventually have that moment of needing to use the facilities and having a nursling who just will not wait). Your mobile nursing kit should include anything you think you might need when you're sedentary and unable to get up for 20-40 minutes.
In our kit, we have:
- A water bottle (nursing moms need about half their body weight in fluids each day)
- High protein snacks
- Fresh fruit
- Reading material
- Chargers
- A phone
- A burp cloth
- A pencil and sticky notes
- Breast pads
- Nipple cream (in this case our favorite go-to: plain cold-pressed coconut oil)
If you have a toddler or preschooler at home already, make them their own mobile play kit. This gives them something so they can occupy themselves while you're nursing, wherever you are nursing. Change the toys or activities out every few days to keep it fresh and boredom-free.
The Bathroom
 Your time in the bathroom might be limited once you're a new mom. It also won't likely be behind closed doors. Still there are some things that need to be taken care of. Once baby is here, your uterus continues sloughing off lochia for a few weeks. This might look like a heavy period for a week or two and tapers off as your body heals. If you're being too active, you might notice the flow increases. If this happens, listen to your body and slow down (moms with stairs might want to consider having a changing table on each floor of the house to minimize stair climbing postpartum). Aside from bleeding, there might be swelling and soreness. Pushing too hard during labor might have caused hemorrhoids, which are uncomfortable and need to be kept clean to heal properly. If you tore and needed stitches this will have some extra discomforts as well. It's important to keep the tools you'll need in any bathroom you might be using regularly or have a mobile basket, lest you need to run through the house with your pants down trying to find what you need (don't worry, we've all been there).
Your time in the bathroom might be limited once you're a new mom. It also won't likely be behind closed doors. Still there are some things that need to be taken care of. Once baby is here, your uterus continues sloughing off lochia for a few weeks. This might look like a heavy period for a week or two and tapers off as your body heals. If you're being too active, you might notice the flow increases. If this happens, listen to your body and slow down (moms with stairs might want to consider having a changing table on each floor of the house to minimize stair climbing postpartum). Aside from bleeding, there might be swelling and soreness. Pushing too hard during labor might have caused hemorrhoids, which are uncomfortable and need to be kept clean to heal properly. If you tore and needed stitches this will have some extra discomforts as well. It's important to keep the tools you'll need in any bathroom you might be using regularly or have a mobile basket, lest you need to run through the house with your pants down trying to find what you need (don't worry, we've all been there).
In our cupboard, we have:
- A peri-bottle, for a bidet-like rinse (a spray bottle will do too)
- Postpartum sitz bath herbs to help with swelling, soothing and healing (we make a concentrated tea to add to peri-bottles or you can use it in a sitz bath)
- Sanitary pads (you'll want heavy duty ones for at least the first few days)
- Bottom balm and bottom spray (in case you don't want to DIY with herbs)
- Witch hazel for help with swelling and itch (put some on sanitary pads to have in the freezer for the immediate postpartum)
- Large wipes for cleaning or using as a compress with sitz bath herbs or witch hazel
- A towel
- Reading material (should you get a few extra moments)
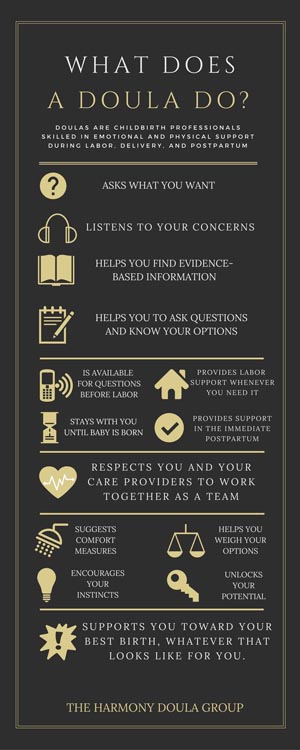
What Does a Doula Do?
We absolutely do the items listed in the graphic. We do all of this and more.
I love birth. I'm addicted to watching a baby grow and decide when to be born. The tremendous privilege of supporting a birthing parent through the powerful stages of labor and encouraging her to push that new life into the world overwhelms me. So to does the indescribable feeling of being present to witness the miracle of birth.
As doulas, we are honored to be a part of all of these stages of pregnancy, labor, and birth. We are there to listen, not just to concerns, but to struggles, to celebrations, to past experiences, and to the wonder of the future. We support the birthing parent mentally, emotionally, and physically before, during, and after the birth. We also hold space, as we say, allowing parents the time and silence they need to listen to their instincts and what their body is trying to tell them. Most people have become unaccustomed to listening to their inner voice, their intuition, and so this holding space is one of the most important things that we do to help them find themselves as parents.
Pregnancy, labor, and birth mainly focus on the birthing parent and baby. But what about the partner? Fifty years ago, the partner was not even allowed into the delivery room. Now we expect that same person to be the expert when making decisions and providing support. This expectation of someone who may have never seen the birth process is hardly fair. As a doula, we value the partner as an integral part of the birthing process. We provide education before the birth, and reminders during the birth, of their game plan. We support the partner physically, reminding them to eat and sleep. We support them emotionally providing an ear and reassurance when all looks well, and an ear and shoulder when they are worried. We whisper suggestions in their ear when they have run out of supportive ideas.
The Harmony Doula Group is committed to being continuously there during the labor process, but we are also available before labor starts. We are there for texts and phone calls, emotional support and education before the birth. We are there during your labor from the moment you need us until an hour or so after the delivery of your beautiful child, providing continuous support when the nurses and doctors cannot. We are there after the birth encouraging bonding and breastfeeding if desired. We are available for that physical and emotional support after the baby during your postpartum home visit. And we are still available by phone and text afterward for a time if you just need to talk.
What does a doula do? We support, encourage, listen, educate, hold space, whisper, stay present, and adapt to the needs of our clients. In his research findings on labor support, Dr. John Kendell has said that "if a doula were a drug, it would be unethical not to use it." We love our jobs and our clients. We are honored to be a part of something so intimate in their lives.
- Susan Jessee
